Is it wrong to use a dead man’s sperm?
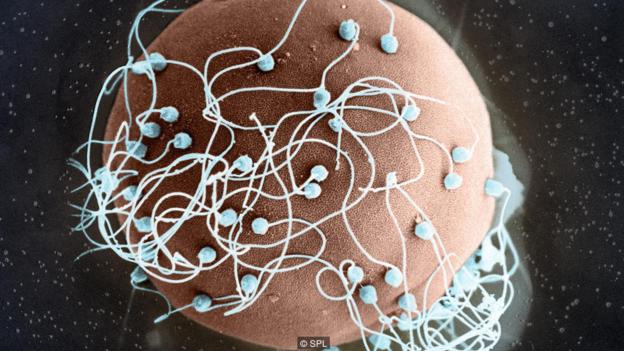
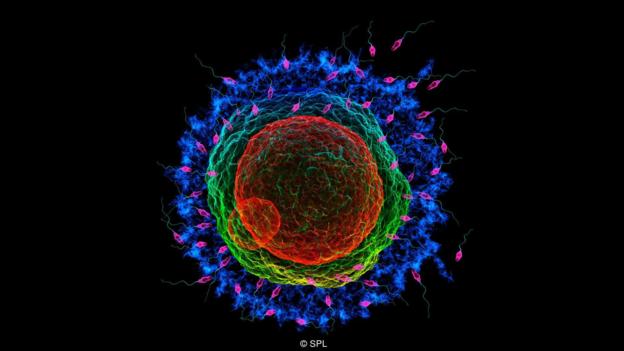
colour enhanced scanning electron micrograph (SEM) of sperm surrounding a human egg. Magnification: 480x.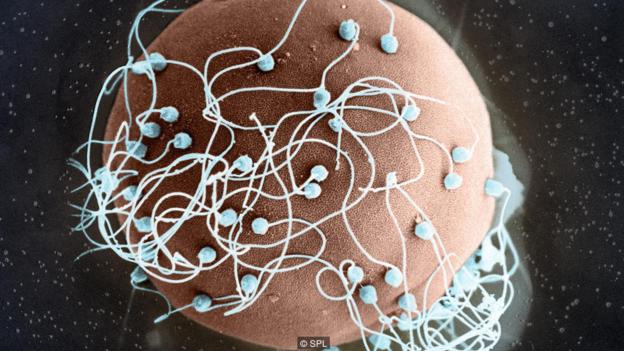
What drives the partners of men who have died to try and have their babies? Jenny Morber delves into the legally and ethically fraught world of post-mortem sperm donation.
There is a man waiting for the doctor and his time is running out.
It is late evening, just over an hour after the doctor first groped for his ringing phone. “Can you help us?” the woman on the other end had asked, her voice breaking.
Now, preparing for the procedure, the doctor is alert. He moves quickly. He scrubs his hands and arms with soap and snaps on his gloves. His assistant clinks down sterilised instruments onto a stainless steel table. The air is cool and heavy with the scent of disinfectant.
The doctor sits over the patient ready to perform the surgery. He pauses, fixing a picture in his mind, then slices through the skin until he can see the organ’s outer layers. It glistens, milky white and veiny. The doctor cuts off a spongy piece and drops it into a vial. His assistant whisks it away.
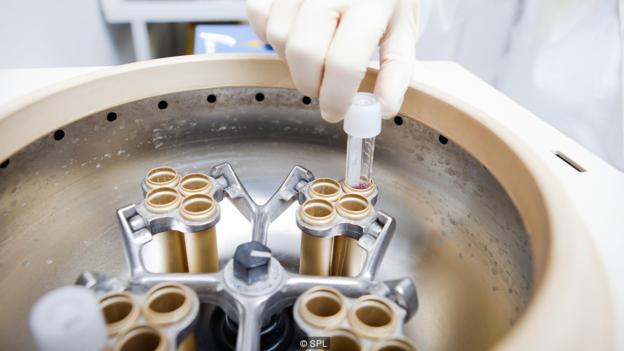
MODEL RELEASED. Sperm bank. Laboratory worker placing a sperm sample in a centrifuge. The sperm is liquified, filtered and centrifuged, causing the seminal plasma to separate from the sperm cells. This work is being carried out at Cryos International Sperm Bank, Aarhus, Denmark. The world’s largest sperm bank, it has stocks of over 170 litres of sperm (around 130,000 samples) that are used for fertility treatments, creating more than 2000 babies each year. Photographed in 2012.
The doctor carefully sutures the patient back up. The room is quiet. There is no beeping monitor or IV drip. No one checks the patient’s vitals. He has been given no pain relief.
The patient is dead.
He has, in fact, been so for a while – over 30 hours, according to his chart – but some of him survives. What the doctor has extracted is a liquid that can create life. An incredible substance that is neither person nor property; simultaneously so abundant yet valuable that we still haven’t quite figured out how to treat it. It is the dead man’s sperm.
A second chance
Ana and Michael Clark had only been married a year when Mike got orders to ship out overseas for his fifth deployment. Mike, 25, was a sergeant in the Marine Corps.
He joined at 18 and in his seven years had already earned several ribbons and medals, including a Purple Heart. The couple had decided to connect with a trip before Mike’s deployment: a motorcycle ride along a California highway.

^BSperm^b ^Bbank.^b Samples of cryogenically stored sperm being removed from the storage tank. This container is filled with liquid nitrogen, which keeps its contents at almost -200 degrees Celsius. After a sample is removed and thawed, the most healthy sperm cells are selected by a computer imaging system and then used for in vitro fertilisation (IVF) to treat infertile couples. Storage of frozen sperm can preserve a man’s ability to have children if his fertility is threatened by cancer of the testis. Use of sperm from an anonymous donor can also help couples where only the male partner is infertile.
It would be their last together. On the way back onto the highway after lunch, Mike lost control of their bike and they flew off a cliff. Ana survived the accident. Mike did not.
Recovering from spine and shoulder fractures in the hospital, Clark was grieving for not only her husband, but their future children. “We had talked about it maybe a week or two before he passed because he was going on the deployment, and he said, ‘Yeah, you know it’s too bad that we can’t go to a sperm bank now and freeze sperm… I have way too much to do at work.’”
It took a few calls before she found a doctor willing to perform a sperm extraction on a deceased patient
Seeing Clark distraught over her lost chance at children with her husband, a friend suggested that she consider retrieving some of Mike’s sperm. “I looked online and called the number for the sperm bank,” says Clark. It took a few calls before she found a doctor willing to perform a sperm extraction on a deceased patient. “And then I had to hire a hearse…”
The hearse took Mike’s body the 100 or so miles from the hospital in Riverside to San Diego for the procedure, and back again.

MODEL RELEASED. Sperm bank. Laboratory worker selecting frozen sperm from liquid nitrogen storage for packaging and shipment. This work is being carried out at Cryos International Sperm Bank, Aarhus, Denmark. The world’s largest sperm bank, it has stocks of over 170 litres of sperm (around 130,000 samples) that are used for fertility treatments, creating more than 2000 babies each year. Photographed in 2012.
Over the phone, Clark comes off as independent and level-headed. Articles in the media sometimes hint that women interested in creating what is sometimes known as a posthumously conceived child are a little off, still clinging to the loved one they can never get back, not quite in touch with reality. Ana Clark’s feet seem firmly planted.
“It gave me a sense of hope that he wasn’t going to be gone forever, that I was going to be able to have a piece of him that was still alive. Just for me. My very own little piece of my Mike.” More than that, Clark wanted Mike to have a legacy. “He was a very, very good man. He was a very good Marine, and to know that I would be able to carry a form of legacy, someone that was going to continue the path as the hero he was, I think that’s what really motivated me…”
Producing the goods
In the late 1970s, Los Angeles urologist Cappy Rothman performed the first post-mortem sperm retrieval.
Before this, Rothman had been extracting sperm from men living with infertility, work that gave him a detailed knowledge of male reproductive anatomy, experience in sperm extraction and preservation, and contacts who knew he was interested in assisting men with reproductive issues.
“Within six weeks of practice, I was booked up for six months,” he recalls. Then, when a prominent politician’s son was left brain-dead after a car accident, “I got a call from the chief resident of neurosurgery at UCLA and he said, ‘I have a strange request. [This politician] would like to have his son’s sperm preserved. Could you do it?’”
Rothman came up with three options: administer a drug that would make the entire body convulse, hopefully inducing ejaculation; remove the man’s reproductive organs and go looking for sperm; or manual stimulation. “I remember there was a pause at the end of the phone… [the neurosurgeon] says, ‘Hey doc, I’ve been asked to do a lot of things as chief resident of neurosurgery but if you think I’m going to jerk off a dead man you’re crazy.’”
They decided on the second option. “It almost felt like Michelangelo,” says Rothman, “being alone, in an OR, with the male anatomy. It was an education.”
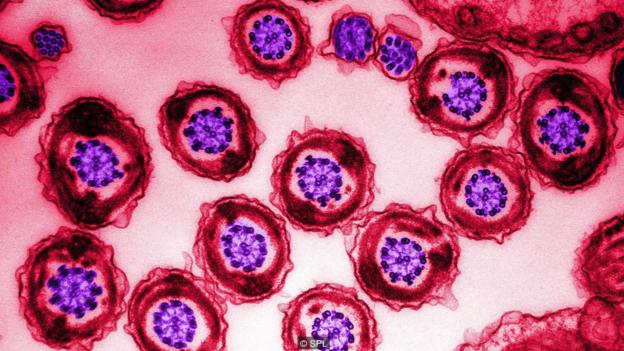
Colour enhanced transmission electron microscope of a cross section of human spermatozoa. A sperm’s tail’s ability to move is partly due to the arrangement of microtubules (part of the cell’s cytoskeleton) within the tail. The microtubules are arranged in a central axoneme with two central single microtubules and nine peripheral double microtubules. Surrounding the microtubules are dense fibers, which provide rigidity and protection to the tail. Next is a layer of mitochondria which provide the energy for movement. Finally the tail is wrapped in a protective outer sheath.
The first live birth resulting from a post-mortem extraction wasn’t until 1999. Gaby Vernoff gave birth to baby Brandalynn from sperm extracted by Rothman 30 hours after her husband died. According to Gaby, the pregnancy took with the last vial of sperm.
Today, Rothman is co-founder and medical director of California Cryobank, the largest sperm bank in the US. He estimates that the practice has performed close to 200 post-mortem sperm extractions. Their records show just three extractions in the 1980s and 15 in the 1990s. But from 2000 to 2014, they performed 130: an average of just under nine a year.
Rothman’s is by no means the only clinic that offers this service. Recent statistics are scarce, but surveys of US fertility centres in 1997 and 2002 found increasing numbers of requests for post-mortem sperm retrieval, although from a very low base.
Life after death
Our bodies, it seems, die not all at once, but in parts. Early scientific literature advises doctors to extract and freeze a sperm sample within 24–36 hours of death but case studies show that under the right conditions, viable sperm can survive well beyond this deadline. Rothman tells of a man who died kayaking in cold water whose sperm were in good shape a full two days later. And in April 2015, doctors in Australia announced a “happy, healthy baby” born from sperm removed 48 hours after the death of the father.

In vitro fertilisation. Light micrograph of a micro-needle (right) that is being used to inject a human sperm cell into a human egg cell. The tip of a micro-pipette (left) is holding the egg cell in place. This in vitro fertilisation (IVF) technique is known as intracytoplasmic sperm injection (ICSI). The injected sperm fertilises the egg and the resulting zygote is then grown in the laboratory until it reaches an early stage of embryonic development. It is then implanted in the patient’s uterus, where it develops into a foetus. IVF allows infertile couples to conceive a child.
The sperm don’t have to be zippy and perfect, just alive – sluggish sperm can still create a pregnancy. All it takes is a single sperm injected into an egg.
But first someone must retrieve it. There are several ways that sperm can be harvested, including needle extraction. As the name suggests, this method involves inserting a needle into the testis and drawing out some sperm.
A second approach is to extract the testis or epididymis surgically. As the epididymis is where sperm go to mature, this tissue is a popular target. The doctor surgically removes the epididymis and milks it or otherwise separates the sperm from the tissue.
Another option is rectal probe ejaculation, also known as electroejaculation. The doctor inserts a conductive probe into the man’s anus until it is next to the prostate. A jolt of electricity causes a muscle contraction that stimulates ejaculation of sperm through the usual channels. Because it does not require intact reflexes, it is also used for men who have spinal injuries.
But just because we know how to extract sperm after death, there is no assurance that someone will be given access to the procedure should they request it. Martin Bastuba, founder and medical director of Male Fertility & Sexual Medicine Specialists in San Diego, is the doctor who retrieved Mike Clark’s sperm after his motorcycle accident. “There are no specific rules,” Bastuba says.
Just because we know how to extract sperm after death, there is no assurance that someone will be given access to the procedure
The US legal position is a tangle of confusing and sometimes conflicting regulations. The laws that govern tissue and organ donation are federal, but they don’t necessarily apply to sperm, classed as renewable tissue. Meanwhile, artificial reproduction is regulated by individual states.
If a man has made no prior directives, such as enrolling as an organ donor, the next of kin can decide when to stop life support, whether to donate a man’s organs, how his body will be used or disposed of, and his funeral rites. But his sperm are often treated differently.
Sperm, it is said, are special. Several recent court rulings have given sperm a legal status higher than that of blood, bone marrow or organs. While those substances and body parts may be used to save life, sperm – like eggs – are often singled out for their potential to create life. In line with this view are positions such as that of the American Society for Reproductive Medicine, which argued in 2013 that, “in the absence of a written directive, it is reasonable to conclude that physicians are not obligated to comply with either request [for sperm extraction or use of extracted sperm] from a surviving spouse or partner”.
Other opinions and legal rulings vary, though. In 2006, a judge who was interpreting organ donation policy ruled that organs, sperm included, can be gifted by a man’s parents after his death, provided the man didn’t previously refuse to make such a gift.
Because we still can’t decide on what sperm are or are not, policies on post-mortem sperm extraction differ between hospitals. Many hospitals have no policy at all.

The American Society for Reproductive Medicine’s position is that post-mortem sperm requests should be granted only to surviving spouses or life partners, and that there must be a grief period prior to the sperm’s use. Notably, it counsels that medical centres “are not obligated to participate in such activities, but in any case should develop written policies”.
If a doctor or hospital does not feel comfortable performing the procedure, often they can release the body to someone else. Bastuba has harvested sperm in the intensive care unit of a hospital, in a morgue, in a medical examiner’s office, and even in a funeral home.
International quagmire
What about other countries? Some have laws in place. Some don’t. Some are permissive. Some aren’t. It’s a global mess.
France, Germany, Sweden and Canada are among the countries that prohibit posthumous sperm retrieval. In the United Kingdom, it is not allowed unless the man has given prior written consent. In the mid-1990s, the case of Diane Blood brought the issue into the public eye. Blood and her husband Stephen had already begun trying for a family when Stephen died suddenly from meningitis. At first the courts denied Blood’s request to have children using Stephen’s sperm, saying its collection had been illegal. But after appeal, she won the right to send the sperm outside the UK so she could undergo insemination in a more permissive country. Blood eventually gave birth to two boys with her husband’s sperm.
Beth Warren recently won a legal battle in the UK to prevent her husband’s sperm from being destroyed following his death. He had banked sperm before beginning cancer treatment and later died from a brain tumour. Regulations had stipulated that the sperm could not be stored beyond ten years without renewed consent.

Medical team preparing equipment for surgery in operation room
In Queensland, Australia, a woman was denied the right to harvest and freeze her husband’s sperm after his unexpected death, although they were planning to start a family. She later learned that her husband may have donated sperm when he was a student.
In Israel, implied consent suffices – a deceased man need not have left a written document, but his widow just has to say that she believes he would give consent were he alive to do so. The government may even provide financial assistance: state health insurance will pay for as many IVF cycles as needed to produce two babies.
Israel’s relatively permissive policies have recently created a rather tricky situation.
The Times of Israel reported in 2015 that parents of a combat reservist killed in training have won the right to have his grandchild. But there was a twist. They won rights to the sperm despite the fact that their son’s widow refused to have his baby after his death and objects to his parents’ efforts to use the sperm themselves.
So how do doctors and review boards weigh up decisions on post-mortem sperm extraction? “Like most issues in reproductive ethics or medicine in general, your big concerns are respecting the wishes and consent of the patient,” says Elizabeth Yuko, a bioethicist. “In this case, because the patient is deceased, this makes it a little trickier, but you also want to respect the welfare of the future child… In a lot of cases you are guessing what the wishes of the deceased are.” Where a man has made his wishes clear, the rights of the dead almost always supplant the rights of the living.
Where a man has made his wishes clear, the rights of the dead almost always supplant the rights of the living
One place where living men are asked about the fate of their sperm after death is at a sperm bank. In 2012 a group of researchers explored this data. Of around 360 men with cancer or infertility diagnoses who banked sperm at a Texas sperm bank, almost 85% consented to post-mortem use.
In a US telephone survey published in 2014, researchers asked people whether or not they would want their spouse to be able to use their sperm (or eggs) after their death to make a child: 70% of men aged 18–44 said yes. The researchers concluded that a presumption of consent would result in the dead men’s wishes being honoured three times more often than the current conservative standard.
Changing opinion
Over the last four decades, attitudes towards the issue seem to have changed.
A 1998 British Medical Journal article discussing the ethics of sperm retrieval said: “Doctors have… unwittingly sanctioned the use of dead men’s bodies for women’s gratification.” The article concluded that doctors “must find the courage to say no to assaulting vulnerable, brain dead patients”.
But in 2008, a survey in a southern state of the US found that “overall attitudes and… beliefs were primarily in favour of posthumous harvesting”. And in 2015, ethicists in Australia published a commentary supporting a presumption of consent on the part of the dead man.
But what about the children? Some feel that posthumous sperm donation should be prohibited in part because it creates disadvantaged children who will never know their biological father. But many children never know their biological father, even if he is alive. “What I found hard to grasp,” says Diane Blood, “was that I could have the sperm of an anonymous donor, even one who was dead, but not my own husband.”
Julianne Zweifel, a clinical psychologist and an ethics committee member at the University of Wisconsin School of Medicine and Public Health, disagrees. “Adults are making a decision to bring a child into the world with, by definition, a deceased parent because of adult needs and not sufficient concern is being paid to what is the impact on the child,” she says.
Four children born from posthumously acquired sperm have shown normal health and developmental outcomes
Zweifel worries about the burdens placed on a child created through loss. “That child can end up being what some people would call a memorial candle to the deceased person… That child can feel that people are looking for traits of the deceased parent in them and they can feel beholden to do that.”
As for evidence, there is very little research on the possible psychological or health effects on a child conceived using sperm extracted posthumously. In 2015 an admittedly tiny study found that four children born from posthumously acquired sperm “have shown normal health and developmental outcomes”.
After everything – the illness or trauma that causes a man to die, the decisions around whether to try to get sperm or not, the processes and procedure involved if you do decide to – the surprising thing is, most relatives never even use the sperm.
The surprising thing is, most relatives never even use the sperm
Rothman and Bastuba view post-mortem sperm extraction mostly as an act of compassion for those who are grieving. Of the roughly 200 procedures they have performed, says Rothman, the extracted sperm have only been used twice.
As for Ana Clark, it has now been almost two years since Bastuba collected sperm from her dead husband. Does she still want to have Mike’s child? “Absolutely,” she says. “There is no possibility of me not having this child.”
It is strange to think that there would likely be fewer people questioning the ethics of Clark’s decision if she were to buy sperm from an anonymous donor. But she already met the man she wants to father her children. “I don’t want children with anyone else,” she says, “I only want them with my husband.”
Политика конфиденциальности | Правила пользования сайтом